Download Medicine Through Time Worksheets
Do you want to save dozens of hours in time? Get your evenings and weekends back? Be able to teach Medicine Through Time to your students?
Our worksheet bundle includes a fact file and printable worksheets and student activities. Perfect for both the classroom and homeschooling!
Table of Contents
Add a header to begin generating the table of contents
Summary
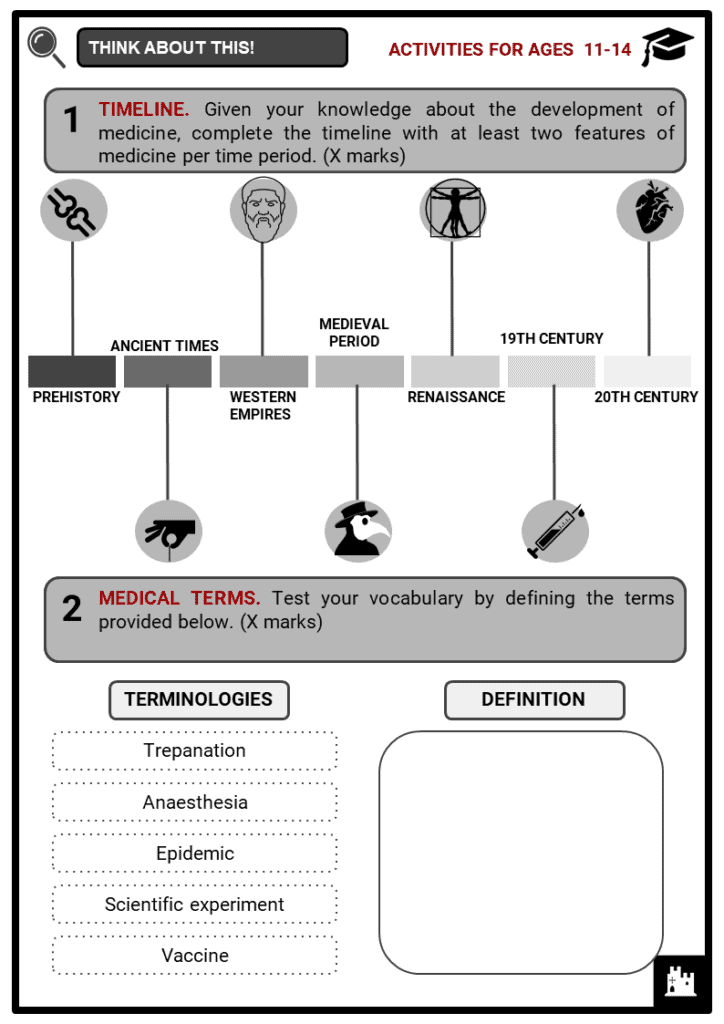
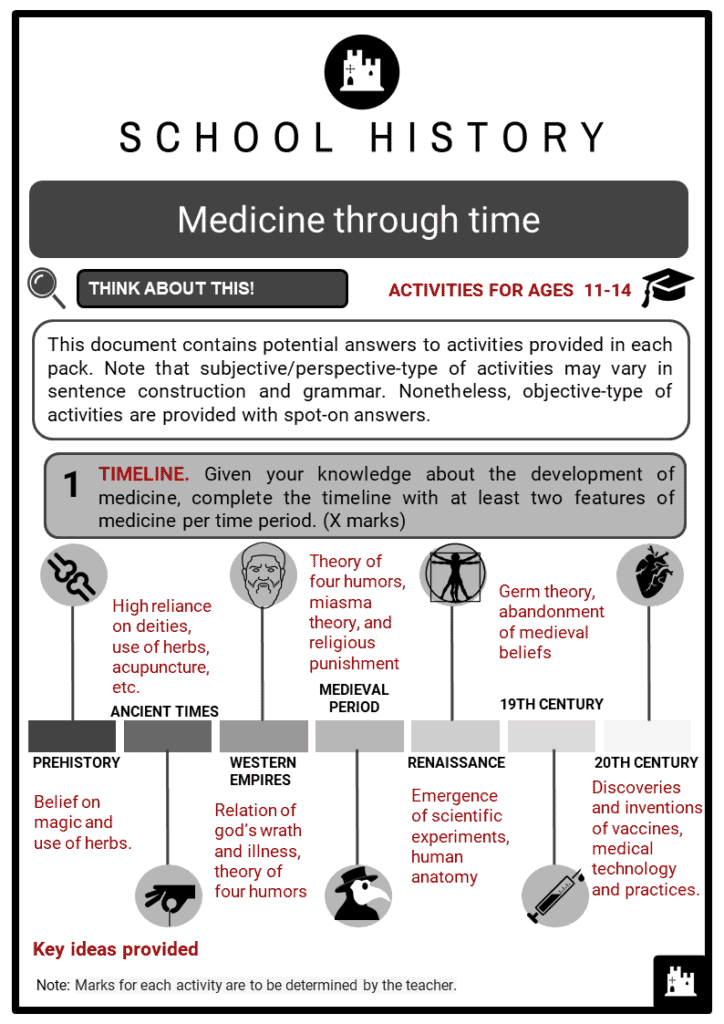
- Brief historical timeline of medicine.
- Features of the field of health and medicine from ancient civilisations until the 20th century.
- Significance of the following events to the development of medicine; (a) Renaissance, (b) Black Death, (c) Industrial Revolution, (d) spread of epidemics, and (e) scientific experiments.
Key Facts And Information
Let’s know more about the development of medicine!
- Medical practice has always existed. Although (naturally) we have few traces of medical knowledge (and phytotherapy) of people from prehistory, we have found skulls of that time bearing marks of trepanation. From two great civilisations of antiquity, the Mesopotamians and Egyptians, come the oldest medical texts known (with the exception of China, whose medicine developed away from Western civilisation, and without mutual influence). Medicine was also found on all continents. It was mainly traditional and practised by many cultures.
Medicine in prehistoric times
- Medical historians suggest that prehistoric people tended to move from one place to another and had no concept of public health. Through archaeological study, prehistoric graves were excavated to rediscover their lifestyle and health. Anthropologists believe that prehistoric humans practised natural and supernatural beliefs in treating diseases.
- Most archaeological evidence (bones) suggests that prehistoric humans were generally healthy but had badly set bones, which indicates that they had little knowledge of how to set broken bones.
- List of diseases or conditions that may have been common among prehistoric humans:
- Osteoarthritis, which may have been caused by carrying large and heavy objects. Strain on the knee joints has been found in bone remains.
- Micro-fractures of the spine probably caused by dragging huge rocks over long distances.
- Hyperextension and torque of the lower back, which may have been caused by raising large boulders.
- Infections from pathogens, as antibiotics and vaccines were not yet known.
- Rickets due to low quantities of vitamins C and D
- Other features of prehistoric medicine
- In prehistoric communities, people believed in medicine men known as shamans. They usually recommended plant-based medicines, including herbs and roots, and spells chanted with charms.
- Medical practices were passed along through word-of-mouth, as most prehistoric communities did not read or write.
- In addition to shamanism, it is believed that they practised geophagy - or the practice of eating earthy substances like clay - to heal external and internal injuries.
- One of the oldest surgical practices concerning the brain was trepanning. A neolithic burial site in France, which is estimated to be about 7,000 years old, revealed the earliest trepanned skull.
- Trephination is a process of drilling a hole in the skull.
- Anthropologists believed that prehistoric humans used trepanning to cure mental disorders, epileptic seizures, and migraines. They suggest that drilling a hole into an individual’s skull would free the victim of demonic spirits, thus curing the disease.
- Based on excavated bones of prehistoric humans, life expectancy among men was between 30 to 35 years old, while women were only between 15 to 25 years old due to the risks of childbirth.
- Ancient people’s understanding of medicine was closely tied to spirits and the supernatural.
Ancient Times: Early Chinese and Egyptian Medicine
- In ancient times, many cultures addressed illnesses with herbal remedies and belief in the supernatural powers of medicine men or witch doctors. Moreover, wearing of amulets and charms was a common practice to heal diseases. For example, ancient Mesopotamians had little knowledge of human anatomy and physiology due to religious taboo. Mesopotamians, therefore, used to dissect animals for divinatory purposes.
Ancient Chinese Medicine
- Based on written records of diseases, ancient Chinese medicine began in the Shang Dynasty. They believed in the basic concept of Qi as the vital force of life. Any imbalance in it caused diseases.
- In ancient times, the Chinese believed that humans and the universe are interconnected with one another. In order to restore balance in the Qi, internal body organs and the external elements of earth, fire, water, wood, and metal needed to be in balance first.
- Like other ancient cultures, the Chinese had little knowledge of human anatomy. Their medicine was based on the cosmic system.
- During the Shang dynasty (1766-1122 BC), people believed that illness was caused by an evil spirit/the devil entering the body, by upsetting an ancestor, or by being cursed.
- Traditional Chinese medicine practised in ancient times
- ACUPUNCTURE is probably one of the oldest Chinese medical treatments ever recorded (about 1600 BC). The practice involves the insertion of fine needles into the skin to stimulate specific points on the body.
- MEDITATION, specifically Taoist meditation, is one of the earliest forms of its kind that brings the mind into a state of contemplation, reflection, and relaxation.
- MOXIBUSTION, or moxa, is a form of ancient Chinese treatment that involves burning herbs near the body. Old texts suggest that this traditional practice was tried if both acupuncture and herbalism failed to heal the illness.
- The use of herbs in teas and powders was one of the traditional ways of treating health conditions.
- Other medical practices also included acupressure, cupping,
tuina, and tai chi.
Ancient Egyptian Medicine
- Ancient Egyptian civilisations believed that physical wellness was connected to spiritual health. Each time the body manifested discomfort or diseases, doctors were convinced that spirits were blocking the body’s channels. In order to solve their problems, doctors (or healers) advised both prayer and natural remedies to their patients. Therefore, it is no surprise to discover that medical roles were filled by priests.
- Their belief in gods, demons, and spirits, blurred the lines between magic and medical, scientific detachment.
- In fact, people believed that illnesses appeared due to the gods’ or evil spirits’ anger: speaking their enemies language of magic and charms could alleviate their patients’ pain.
- In essence, ancient Egyptian civilisations believed that they were afflicted by diseases and pain because they had to learn a life lesson or because they had to redeem their sins.
- Overall, it can be stated that ancient Egyptian medicine was grounded in mysticism and herbology.
- Since the ancient Egyptians had their own alphabetical and numerical system, they recorded their medical findings, and they compiled the Ebers Papyrus, which today is the most ancient text concerning medical practice.
- The book was written around 1500 BCE, and it contains over seven-hundred remedies, charms and incantations that date back to 3400 BCE.
- In ancient Egypt, there existed three types of medical practitioners: priests, magicians or sau (who executed a number of spells and charms in order to get rid of evil spirits), and healers called swnw, who used medication to cure their patients.
- Although the ancient Egyptian civilisation’s knowledge of anatomy was not highly developed, they had reached certain important understandings and discoveries: in fact, they knew that that the heart pumped blood through the veins and arteries, therefore, providing blood to the body.
- They were also aware that the liver could be infected and could suffer diseases, however, they did not know what caused them.
Western Empires: Early Greek and Roman Medicine
- The development of Western medicine was spearheaded by the ancient Greeks and Romans. Initially, the gods were believed to be the ones who sometimes caused diseases, and could also cure them.
Early Greek Medicine
- With the concept of “a healthy mind in a healthy body”, ancient Greeks viewed medicine as the connectedness of both physical and mental health.
- Hippocrates, also known as the ‘father of medicine’, was a Greek philosopher who developed the theory of four humors or liquids that remained popular in Western Europe until the 17th century.
- In addition to the Hippocratic School of Medicine, Hippocrates pioneered the examination of a living person as a means of studying diseases.
- Today, the Hippocratic oath is widely used by doctors and other healthcare professionals as a commitment when practising medicine.
- In addition to Hippocrates, Aristotle and Plato also concluded that the human body had no use after death, in contrast to ancient beliefs of the afterlife.
- Moreover, Thucydides concluded that incantations and prayers were an ineffective way to cast out diseases and plagues.
- The theory of the Four Humors states that the human body is composed of four substances or liquids that should be in perfect balance, if not, sickness will occur.
- Succeeding generations further developed the theory of the four humors.
- Galen, a Greek-born Roman citizen and supporter of Hippocrates who lived centuries after, expanded humoral physiology.
- He included the three varieties of pneuma or vital energy: the liver, heart and brain.
Early Roman Medicine
- The early medicine of the Romans was almost exclusively based on magic. They worshipped a remarkable array of highly specialised medical deities. Unlike the Greeks, the Romans had less regard for the medical profession. After Julius Caesar granted Greek physicians Roman citizenship, the prejudice against them eventually diminished and doctors became popular, famous and rich.
- In the 2nd century CE, Aretaeus of Cappadocia, a follower of Hippocrates, wrote descriptions of several diseases including tetanus, epilepsy, hysteria, and asthma. Moreover, it is believed that he was also able to provide important distinctions between acute and chronic disease, as well as between infections and contagion.
- Another great Roman encyclopedist was Aulus Cornelius Celsus. He prepared eight extant books entitled De re medicina, and many diseases, such as Celsus’ chancre, Celsus’ vitiligo, Celsus’ papules, which still bear his name. Celsus introduced the use of such terms as heart disease and insanity. His descriptions of inflammation, meningitis, and appendicitis are still of great value.
- Beliefs, remedies and domestic medicine
- Authentic Roman medicine was administered by the pater familias (the father of the house), who cured his family by using wine, oil, and wool.
- According to Cato, illnesses were considered a test: in fact, a person demonstrated her strength if she managed to overcome her sickness through the remedies offered by nature.
- Despite the traditionalists’ distrust, Greek and other foreign doctors became so popular in Rome that both Caesar and Augustus granted them the right to Roman citizenship and forbade that they could ever be sent back to their countries of origin (Suetonius Iul., 1; Aug.,42, 3).
- The medical profession was profitable, and many completely inexperienced people (such as cobblers and weavers) became doctors overnight. In essence, these untrained people became doctors by directly learning and experimenting on their patients. Some of the most ignorant and lethal doctors were put on trial.
- When surgical operations were carried out, patients were more or less narcotised, and the surgeons’ assistants held them down while the doctor operated.
- Bloodletting was also used as a remedy for many diseases.
- Like the Greeks and the Egyptians, the Romans used various religious rituals for healing, since they believed in the supernatural origin of many diseases.
- However, Rome also developed sanitary services intended to prevent diseases. For instance, they attempted to introduce more healthy environments with the construction of aqueducts that could supply water to the city.
Medieval Medicine
- Historically, the Medieval period in Europe began with the fall of the Roman Empire, thus making medical knowledge derived from the ideas of Hippocrates and Galen. In general, societies during this period carried out medical practices that today are considered unhygienic, hazardous, and unreasonable.
- The superstition and dogmatism that marked the rise of Christianity in Europe continued to flourish throughout the Middle Ages.
- As in Babylon, astrology ruled the prognosis as diagnosis was largely limited to an inspection of the urine. Free inquiry, observation, and experiments were out of the question; learning, including magical learning, was devoted to the study of the ancient authoritative texts.
- Therapy relapsed into magic and prayer, fantastic and often revolting concoctions, charms and amulets, and faith healing.
- Venesection and various herbs were used widely. Dissection of cadavers was completely forbidden, and anatomy, if studied outside of textbooks, was based on the dissection of pigs.
- Hygiene and sanitation were at a very low level, since the human body was held in contempt - being a temporary vessel that housed the soul.
- The demonic theory of disease gained ascendancy, or else, as in the case of the devastating plague epidemics, the blame was placed on the Jews.
- Throughout the Middle Ages, only the wealthiest could afford physicians. On the other hand, the poor were obliged to consult local practitioners that referred to folkloric traditions.
- Medieval Epidemic: The Black Death
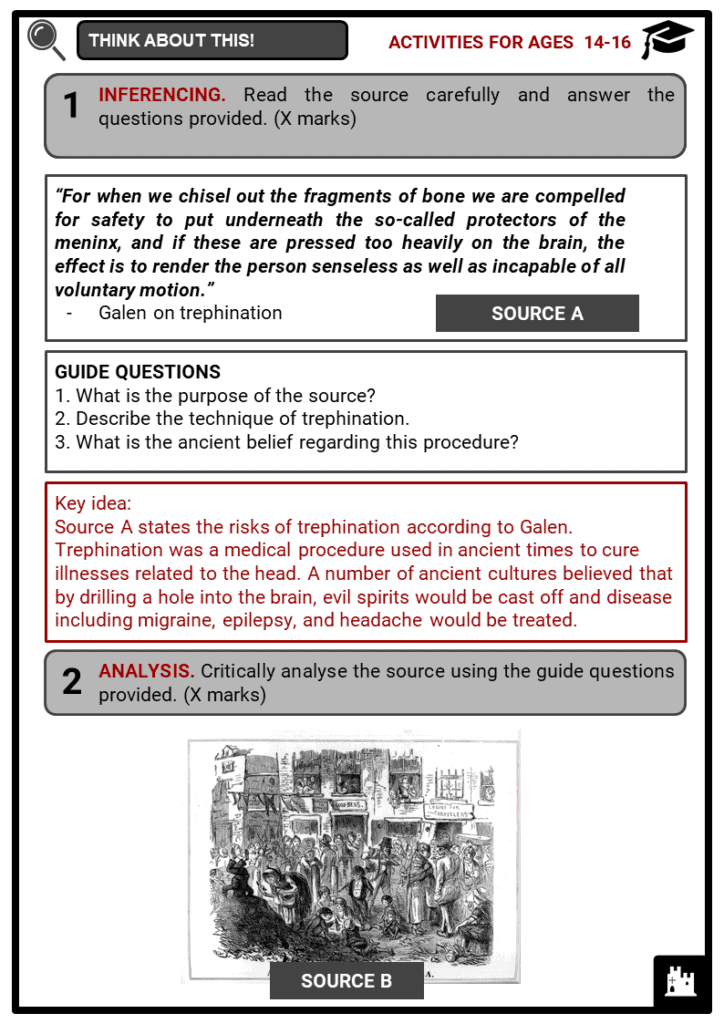
- When the bubonic plague started in Europe due to widespread unhygienic habits, people were not aware that the main cause of death was the bacteria Yersinia pestis, which was spread by infected fleas on black rats.
- Not having a scientific explanation for the disease that had wiped out over one-third of Europe’s population, people attempted to save their lives in a variety of ways.
- In an age when religion ruled society and its thought, it is not surprising that the Black Death was considered a sort of divine punishment inflicted by God on sinful members of humanity. In fact, some Christians that believed such theory punished themselves severely through self-flagellation.
- Others thought that the best solution to avoid the plague was hiding in the sewers, where no one could reach them, see them, or touch them.
- However, the filthy conditions of the sewers, with their foul-smelling surroundings and fetid insects, did not save them from death: and although they may not have been infected by the bubonic plague, they nonetheless died due to other severe illnesses and infections.
- Several medical practices and beliefs during the Middle Ages
- If an individual suffered from regular headaches, migraines, or epilepsy, trepanation was carried out: such practice consisted of perforating the skull with the intention of relieving pressure.
- Stomach problems were cured using herbal remedies. One of them was St. Paul’s potion, which involved the use of several ingredients such as: ‘liquorice, sage, willow, roses, fennel, cinnamon, ginger, cloves, cormorant blood, mandrake, dragon’s blood, and three kinds of pepper’ (Tan 2016).
- Teeth were cleaned with a cloth or with leaves. In cases of decay, they were extracted by local barbers.
Renaissance Medicine
- The main factor that contributed to Renaissance medicine was increased anatomical knowledge. Societies eased the religious and legal restrictions that had been put on dissecting cadavers. This allowed physicians to carry out many anatomical studies, making a lot of new discoveries about human anatomy possible.
- Medical practices and development during the Renaissance
- Autopsy was first introduced by the Greeks in Europe, but was immediately halted with the rise of the Church. Leonardo da Vinci had several accounts on dissection of the human body, while Giovanni Battista Morgagni led autopsy in science form.
- Today, autopsy is a general procedure of finding out the cause of death.
- Trepanation was a surgical procedure in which a hole is drilled into the skull to treat intracranial ailments. The screw-like saw and holder were believed to treat seizure and mental disorders.
- Bloodletting using leeches became a prominent practice in the Renaissance era until the 19th century. Based on the theory of humors, blood’s imbalance was pointed out as the cause of headache, fever, apoplexy, and others. As a cure, blood was drawn until the patient began to faint.
- Accounts showed that C-section was used in the Renaissance era as an extreme and rare approach for child delivery. During Medieval times, the high mortality rate of C-sections made it unpopular. It was only in the 20th century when this method improved and was accepted worldwide.
- Other practices included maggot therapy, cauterisation, tracheostomy, enema, catheterisation, faecal transplant, and cataract surgery.
19th-century medicine
- The Industrial Revolution had a profoundly transformative effect on public health. Overall, it has been concluded that while the Industrial Revolution brought with it a lot of widespread health issues, it also led to major improvements in public health and facilitated the formation of the basis of what we today call public healthcare.
- Scientists had finally made the link between microbes and disease, and chemists had found a way to use particular gasses as anaesthetic.
- Anaesthetic
- Patient comfort during and after surgery drastically improved. More effective anaesthetics meant longer surgeries were possible.
- Germ Theory
- New understanding that bacteria caused decay and diseases meant efforts were directed into finding compounds that killed them.
- Antiseptic breakthrough
- The introduction of the antiseptic carbolic acid during surgery proved the necessity for sterile instruments, clothing and clean theatres.
- Blood transfusions
- Blood groups were discovered in 1900 by Dr Karl Landsteiner, meaning successful transfusions could be given during and after surgery.
- Spread of epidemics and medicine breakthroughs
- Among the key public health issues that gave way to development in medicine during the Industrial Revolution was the spread of epidemics, such as cholera, typhoid, typhus, smallpox, and tuberculosis.
- Following a serious outbreak of typhus in 1838, Edwin Chadwick convinced the Poor Law Board to investigate. He used doctors to give feedback about whether the conditions of the poor contributed to disease prevalence in their communities.
- John Snow established that cholera was waterborne by mapping out cases in Broad Street, Soho, London, which led to a single contaminated well. Further investigation revealed a cracked cesspit nearby was contaminating the water supply. Snow pressured water companies to clean up their water supplies.
- Pasteur theorised that if microbes were responsible for souring, then they might be the cause of disease too. He proved his theory by sterilising water and keeping it in an airtight flask while sterilised water in an open flask grew microorganisms.
- Development of the Germ Theory
- Germ Theory is currently the most widely accepted scientific theory for many diseases across the globe. It simply states that microorganisms, known as pathogens or “germs”, which exist in various conditions, can lead to disease. It has roots in the Middle Ages.
- During the Middle Ages, illness was believed to have come from miasma. People argued that the transmission of disease to another was by breath or bad air.
- Supporting Pasteur’s initial theory, Robert Koch came up with his own experiment, which developed the four basic criteria on what particular organisms caused certain diseases.
- His work discredited the early idea of spontaneous generation and presented the foundation for modern medical microbiology.
- Smallpox and Edward Jenner
- Since the Spanish conquest of Mesoamerican civilisations until the 18th century, smallpox was a huge killer. Prior to vaccination, inoculation or variolation was the most known preventive measure to control the spread of this disease.
- Due to expanding trade networks and exploration, smallpox spread on a global scale through the centuries.
- In the early times, variolation was used to prevent the spread of smallpox. Variolation is a process of giving smallpox sores or pustules to people who had never had smallpox. However, as the person developed symptoms of smallpox, a high risk of death existed.
- It was only in 1796 when English physician Edward Jenner observed that milkmaids who were exposed to cowpox did not contract smallpox.
- Jenner then variolated his gardener’s son with cowpox pus. After months of observation, the child never developed smallpox. Amidst opposition, further research and experiments gave way to the development of a vaccine against smallpox.
20th-century medicine
- By the 20th century, discoveries and advances in the field of medicine doubled an average person’s lifespan. As people began to realise that poor standards of urbanisation and sanitation caused diseases, many became conscious of cleanliness.
- Medical inventions and practices
- In 1901, Austrian biologists and physician, Karl Landsteiner identified and classified blood types into groups.
- In 1928, Alexander Fleming, a Scottish pharmacologist, discovered penicillin, the first antibiotic.
- Between 1923 and 1927, vaccines for diphtheria, whooping cough, tuberculosis, and tetanus were created.
- In 1952, American virologist, Jonas Salk came up with the first polio vaccine. He was regarded as a miracle worker for curing one of the most serious public health concern in the US during WWII.
- In 1953, James Watson and Francis Crick discovered the double-helix structure of DNA thanks to Gregor Mendel who had an earlier theory of the principles of single-gene inheritance.
- British geneticist, Sir Alec John Jeffreys developed DNA fingerprinting and profiling in 1985.
- The 20th century was indeed a progressive period in the field of medicine. The challenge of malignant disease such as cancer is still addressed today with therapeutic practices of surgery, radiation therapy and chemotherapy.
Let’s take a closer look!
- The History of Surgery
- The oldest textbook of surgery was the “Sushruta Samhita”, which recorded the interventions of Sushruta, a Hindu doctor of the sixth century BC and the father of this practice. He invented the removal of the prostate, the treatment of ocular cataracts, the drainage of abscesses, and a technique of nasal reconstruction (at the time, the nose of criminals was cut off) consisting of taking skin from the forehead of the patient.
- The earliest evidence of surgical procedures was as early as 3000 BC, during the pre-Classical ages when people used trepanation. Such an ancient practice was used throughout Europe, Africa and South America until the Middle Ages.
- Based on archaeological findings, ancient Mayans used dental surgery for religious and ritual reasons, rather than health. They used precious stones to fill cavities.
- In the West, ancient Greeks performed surgical procedures like amputations, setting of broken bones, and bloodletting. However, mortality rates were still high due to infection.
- In the 16th century, Andreas Vesalius, one of the founding fathers of modern surgery, began human dissection for education and understanding of anatomy. In 1543, he published De Humani Corporis Fabrica Libri Septem, which corrected misconceptions based on Greek and Roman ideas.
- By the late 1800s, the use of anaesthesia during surgeries lessened the fear of patients of pain and death. However, infection remained one of the major causes of death until the development of ‘listerism’. This method, named after Joseph Lister, involved the removal of bacteria from surgical instruments.
- In the 20th century, surgical procedures were made bacteria-free through boiling of instruments, using autoclaves and chemical antiseptics. Moreover, physicians and surgeons began to wear clean linen and use sterile operating tables.
- Problems of Surgery
- These are the problems faced by surgeons during those time.
- Despite the long practice of surgery as treatment, this procedure was still considered dangerous and risky in the early 1800s.
- Pain
- Due to a lack of anaesthesia, patients who underwent surgeries could die of clinical shock in the process.
- In order to solve this problem, surgeons tried getting the patient drunk or high on opium.
- The use of chloroform as an anaesthetic was widely accepted when Queen Victoria herself tried it during the delivery of her 8th child.
- Infection
- Without the knowledge of microbes that caused infection, people wore dirty clothes, used unsterilised apparatus and worked on unsanitary tables.
- After the discovery of Germ Theory, antiseptics soon followed. Joseph Lister introduced the use of antiseptic and practise of cleanliness during surgical operations.
- Bleeding
- During surgery, patients could die if they lost too much blood.
- With the discovery of blood circulation by William Harvey, blood transfusions were attempted. Initially, attempts of blood transfer were disastrous since blood groups were not yet discovered. Moreover, the dangers of introducing infection and clotting were present.