Download The Impact of War on Public Health in the 20th Century Worksheets
Do you want to save dozens of hours in time? Get your evenings and weekends back? Be able to teach The Impact of War on Public Health in the 20th Century to your students?
Our worksheet bundle includes a fact file and printable worksheets and student activities. Perfect for both the classroom and homeschooling!
Table of Contents
Add a header to begin generating the table of contents
Summary
- Status of public health during the World Wars
- The establishment of the NHS
- Prominent people who made major contributions in public health
- Effect of World Wars on public health
Key Facts And Information
Let’s know more about The Impact of War on Public Health in the 20th Century!
- As the deadliest and the most globally devastating conflicts in human history, World War I and World War II had a major impact on the development of public health in the 20th century.
- Some of these influences were immediate and others were long term.
- Some were immensely positive, and others were debilitating.
- But the World Wars were not the only conflict to affect public health in Britain in the 20th century. The long and drawn out Second Boer War (1899-1902) revealed health issues in the British army. As a much larger and stronger force, it was not able to defeat the South Africans for a whole three years.
- Therefore, in the wake of the Second Boer War, the Committee on Physical Deterioration was created in 1903 to study the health of the British populace and to determine why so many recruits had been of ill health.
- The Committee on Physical Deterioration’s research paved the way for the 1906 Liberals’ reforms in public health including the first National Health Insurance scheme.
- While they were not in themselves comprehensive or universal in coverage, these public health reforms formed important stepping stones towards more comprehensive ones in the 1940s.
- The main reason the World Wars had such a huge impact on public health in the 20th century was that there were simply many more people to care for than in peacetime.
- The other was that conscription, which began in 1916 during WWI, revealed that the levels of health across the country were still, despite the Liberals’ reforms, very poor.
- Following World War I, the very first Ministry of Health was established, recognising the need for greater government involvement in order to improve social security and public health.
- Healthcare provisions improved greatly in the interwar period.
- In the lead up to WWII, the Emergency Health Service (EHS) was created in 1938. This revolutionised healthcare in Britain by driving hospitals and clinics from across the country to coordinate.
- Throughout the war, several major challenges including the Blitz were tackled by newly coordinated healthcare services, spearheaded by the EHS.
- During the war, William Beveridge released his report on social security in Britain, identifying major challenges in British society.
- One of these was disease.
- The report had a major impact on post-war public policy thinking and formation.
- It began a chain of events and policies that resulted in the creation of the National Health Service (NHS) in 1948.
National Health Service
- The National Health Service, or NHS, is one of the major social reforms that followed World War II.
- It is specifically a healthcare organisation established in 1948 that seeks to provide free healthcare and medical services.
- People who use the NHS are not obligated to pay for its services.
- Employees of the NHS, mostly general practitioners or family physicians, are paid through taxes collected by the government as well as employee contributions from their wages.
- The NHS is divided into four systems under the four countries of the United Kingdom, namely (a) National Health Service in England, (b) Health and Social Care in Northern Ireland, (c) National Health Service in Scotland, and (d) National Health Service in Wales. Each system works differently as they are handled by their respective country.
- The services provided by the NHS consist of hospital and specialist services, local health authority services, and general practitioner and dental services.
- Overall, the services of the NHS have managed to provide healthcare at a low cost.
- As medical technology advanced, however, it became difficult to keep the NHS financially stable as medical equipment became more expensive.
World War I and Public Health
- With the start of World War I, hospitals suddenly had to be transported towards the edges of the battlefield as there were no other means of treating wounded soldiers and civilians.
- For Britain, it was mainly the soldiers that were wounded as the island nation was never itself a battlefield. Having never seen a conflict at such a scale, healthcare professionals (including doctors, nurses and other staff) had never been mobilised at this rate before.
- While World War I is known as the very first of the mass killings of the 20th century, having resulted in the death of over 10 million soldiers alone, the wounded and injured, however, really got to witness and eventually enjoy major achievements and progress in medical care in the 20th century.
- Treatment of soldiers in WWI began with frequent and often needless amputations in 1914 to eventually reaching a stage where soldiers could be transported to a hospital, disinfected, and operated on to eventually make a partial or full recovery.
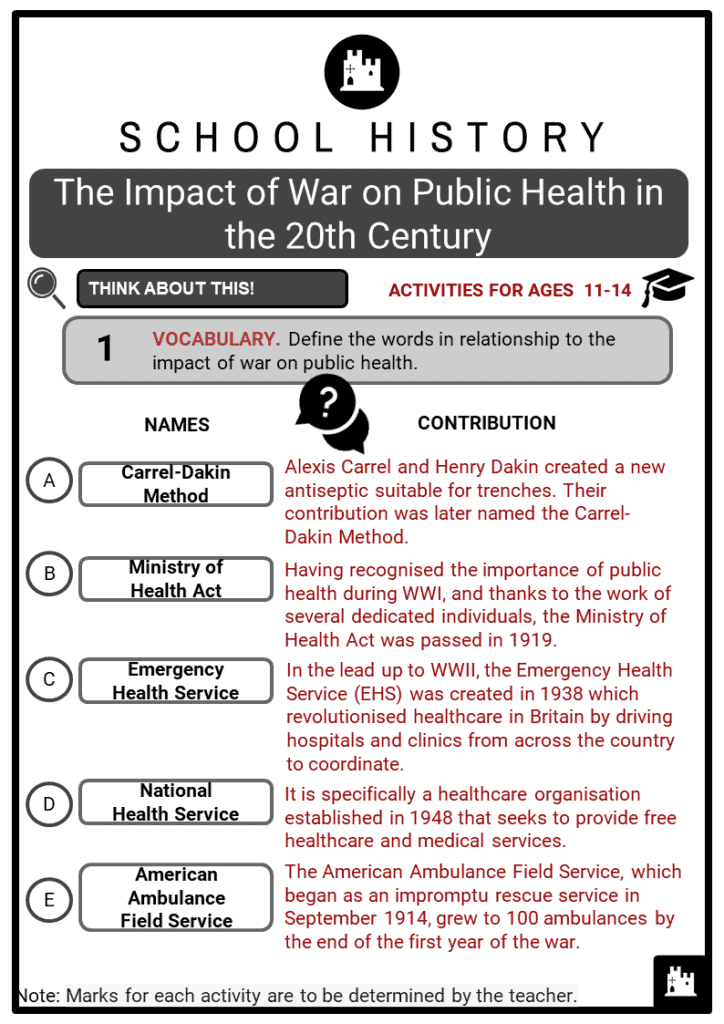
- There were three fundamental elements of healthcare taken for granted today that were born during World War I.
- These were ambulances, antiseptics and anaesthesia.
- In the early weeks of WWI, tens of thousands of soldiers were enduring needless amputations.
- This was, doctors explained, because the trenches lacked the skilled surgeons needed to perform the needed surgeries, and the sanitary conditions necessary to facilitate these treatments.
- In 1915, Professor Théodore Tuffier testified that as many as 70% of the amputations in the trenches had taken place because of infections and not because of the initial injuries on the battlefield.
- This prompted the Rockefeller Institute for Medical Research to contribute the tools and expertise necessary for the creation of new antiseptics.
- With the financial help of the institute, and facilities in a military hospital in France, the French physician Alexis Carrel and Henry Dakin, a British biochemist, created a new antiseptic suitable for the trenches. Soon enough the “Carrel-Dakin Method” was adopted by doctors across Europe.
- Though James Simpson was the first to demonstrate chloroform’s anaesthetic properties, George Crile introduced doctors to a method of anaesthesia, better known as nitrous-oxide anesthesia. He had developed this with a nurse anesthetist in Cleveland named Agatha Hodgins.
- He gave surgical demonstrations using a nitrous oxide-oxygen mix and, while doctors in France were sceptical at first, they eventually saw how effective the anaesthesia was and began asking to use it in hospitals across the country.
- As for innovation on transportation, the American Ambulance Field Service, which began as an impromptu rescue service in September 1914, grew to 100 ambulances by the end of the first year of the war.
- Philanthropists began to donate cars and money and drivers volunteered their services soon enough.
- From 1916, the Red Cross began to supply ambulance cars which greatly supported the war effort.
- Although the so-called Great War had lasted far longer than expected, and had ended in tragedy, several key milestones in medical innovation had been reached, paving the way for major improvements in healthcare in the future.
The Interwar Period
- To make the effects of WWI worse, the masses of civilian and military deaths that happened during the war were followed by an influenza pandemic.
- The 1918 influenza pandemic, also known as Spanish flu (although it did not actually originate in Spain) was one of the deadliest pandemics to date.
- It lasted almost 3 years and infected over 500 million people across the globe.
- Estimates of deaths caused by the influenza range between 50 and 100 million.
- In Britain alone, it is said that 228,000 people died.
- Together, the influenza and the war had ravaged British society, greatly increasing both morbidity and mortality rates.
- As the country struggled to recover from a painful four years, breakthroughs were made in treating pneumonia, which commonly occurred after the influenza virus was contracted.
- More so than just medical innovation, the interwar period allowed the government to take stock and reorganise public healthcare.
- The 1929 Local Government Act ended the division of responsibilities established earlier in the 20th century and dissolved Poor Law Unions.
- Instead, it established Public Assistance Committees in the Country Boroughs and County Councils which went on to take on many ex-Poor Law responsibilities.
- By doing this the act sought to mitigate the stigma which was associated with the Poor Law and its services.
- By integrating medical services, the LGA allowed for many ex-Poor Law infirmaries to be developed into general hospitals that offered acute in-patient care.
- Most importantly, having recognised the importance of public health during WWI, and thanks to the work of several dedicated individuals, the Ministry of Health Act was passed in 1919.
- It gave Britain its very first Health Minister, Christopher Addison.
World War II and Public Health
- By the time that World War II began on 1 September, 1939, Britain’s new Ministry of Health had a couple of decades of work behind them.
- In the interwar period, specialist clinics had been established which treated both common illnesses and advised on nutrition and fitness.
- As fears of war began to rise in 1938, Britain established an Emergency Health Service (EHS) which was tasked with dealing with the aftermath of mass bombing of cities.
- After the war started, the EHS soon became a vehicle for driving cooperation in public healthcare.
- Before WWII, hospitals and clinics had never had to cooperate, share supplies or efforts, nor did they think of themselves as one large organisation.
- The simple matter of need during major devastation in the war like the Blitz and the aftermath of Dunkirk forced British healthcare services to work together, spearheaded by the EHS.
- They were an example of the major challenges that could be tackled, and the major achievements British healthcare could reach if it worked as a coordinated system.
- In many ways this inspired thinking after WWII was behind the creation of the National Health Service (NHS) in 1948.
- Not only did the British government learn from evolving healthcare practices during the war, but they also learned from their own research that greater efforts were needed on their part to better the lives of the British people.
- Infamously, William Beveridge was commissioned to investigate social security in Britain.
- In December of 1942, the Committee’s Report on Social Insurance and Allied Services was published and identified five major problems in British society: want, ignorance, squalor, idleness and disease. Each of these five identified issues, especially the final one, played a major part in the establishment of the Welfare State following the war and the creation of the NHS.
Image sources:
[1.] https://upload.wikimedia.org/wikipedia/commons/c/c8/World_War_I_hospital_patients.jpg
[2.] https://upload.wikimedia.org/wikipedia/commons/0/08/Christopher_Addison%2C_1st_Viscount_Addison.jpg