Download National Health Service (NHS) Worksheets
Do you want to save dozens of hours in time? Get your evenings and weekends back? Be able to teach about the National Health Service (NHS) to your students?
Our worksheet bundle includes a fact file and printable worksheets and student activities. Perfect for both the classroom and homeschooling!
Summary
- History of the National Health Service
- Development of the NHS
- A Modern and Dependable NHS
- The Impact of New Medicines in the NHS
Key Facts And Information
Let’s know more about the National Health Service (NHS)!
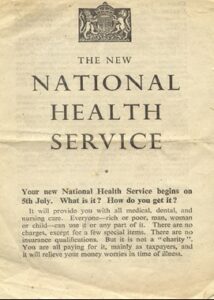
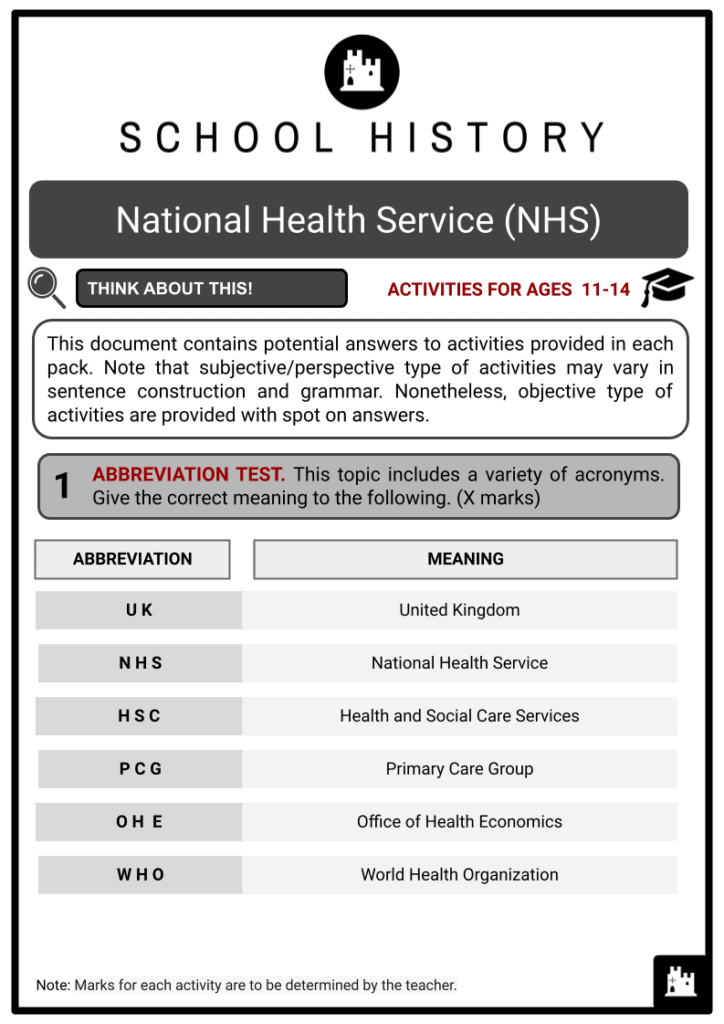
NHS, or the National Health Service, refers to the medical and health care services provided free of charge by the government to all residents of the United Kingdom. The fund is financially supported by the taxes paid by UK residents. This method was also adopted by the Scottish Government, the Welsh Government, and the Northern Irish Assembly. It is not officially known as the NHS in Northern Ireland, rather the Health and Social Care Services (HSC).
The leaflet says, “It will provide you with all medical, dental, and nursing care… There are no charges, except for a few special items… You are all paying for it, mainly as taxpayers…”
History of the National Health Service
- Since its inception, England has had a state-funded health care system, but it was previously monasteries that provided the financial help. However, when King Henry VIII established the newly formed Church of England in 1543 to legitimise his second marriage to Anne Boleyn, he destroyed the monasteries. As a result, the main source of funds for health care, particularly for the poor and vulnerable, was also eliminated.
- Many efforts were made to restore the lost source of funds for the needy. Some of these include Queen Elizabeth I's Poor Law of 1601, the austere workhouses constructed in the 19th century and Lloyd George’s 1911 ‘panel system’, which provided health insurance to all working men.
- The first step towards the establishment of the NHS was taken in 1938. With World War II looming, the government was forced to establish an Emergency Medical Service in which all sorts of hospitals were tolerated and centrally managed to absorb a high number of casualties. This incident gave birth to the idea of establishing a state-funded hospital service, which was made into a reality at the end of the war.
- As a result of the post-war effect, the ministry of health had been considering implementing a health service for the general public. Principles were being analysed, particularly how it would be funded through general taxation. Aneurin Bevan, the next health minister, took on the collaborative ideas. When Bevan became health minister, he made it possible to establish the NHS. Bevan was the one who campaigned for the establishment of the NHS. As a result, he is known as the ‘father of the NHS’.
- The newly formed Labour administration established what is today known as the National Health Service (NHS) in 1948. Its primary goal is to ensure basic personal and social security needs. Since its creation, the essential premise underlying the NHS has been that its services would be paid through general taxation and would be free at the point of use for everyone, regardless of social position.
- “Anyone can use it - men, women, and children. There are no age limits and no fees to pay… Your right to use the National Health Service does not depend upon any weekly payments…”
Development of the NHS
-
Enoch Powell: Founder of the ‘Hospital Plan for England and Wales’ Following the creation of a nationalised health industry, the UK government examined how to administer it effectively during the late 1940s. The principle of managing the NHS was influenced by the practice during the war years. It was especially known as ‘command and control’, where orders were sent down through a chain of command. During the 1950s, they struggled because the service needed more funding than expected.
- The 1960s was said to be a decade of fast expansion. New hospital buildings were constructed, and new medical technology was discovered. A ‘Hospital Plan for England and Wales was made, focusing on the ratio of hospital beds and the population that the NHS served as the basis for planning and constructing hospital buildings. It also instructed those who needed specialised care to be sent to regional hospitals.
- The 1970s were defined by ‘corporate’ approaches towards the health care system. The transition to a population-based funding structure continued, but relations between management and employees deteriorated under the influence of powerful and generally unsatisfied trade unions. This degradation was partly caused by managers beginning to address inefficiencies, but also by requests to correct historically low compensation that proved impossible to deliver.
- By the early 1980s, two major reallocations of financial resources had begun. The first was from one geographical location to another to remedy historical imbalances, while the second was geared at non-acute services. The changes that occurred in the 1980s laid the groundwork for the 1989 health care reforms. Despite managerial simplification and a focus on health promotion and prevention, demand for funds had gradually increased over the previous ten years.
- The advent of an ‘internal market’ for health care was the most significant development. Within this framework, health authorities were tasked with analysing the health of their resident population and procuring the services needed to address recognised requirements from the public or, in principle, private sectors. In contrast, NHS providers that had been created as ‘self-governing’ organisations were able to focus on efficiently providing services.
A Modern and Dependable NHS
- The NHS was in a condition of despair in 1997, after an 18-year period of Conservative governments. Millions of patients, most of whom were on a waiting list, unable to be served due to a lack of staff. Given that the major job of health authorities is to improve people’s health, they also emphasised health service planning and commissioning. The 1997 NHS restructuring, dubbed ‘The New NHS: Modern, Dependable’ enabled these health authorities to concentrate on strategic planning.
- The so-called New NHS included the following recommendations for specific goals:
- To lower transaction costs, abolish the internal market.
- Introduce Primary Care Groups (PCGs), with each group accountable for people’s health care, so that only one budget is allotted to both primary care and prescribing.
- As a longer-term approach to service planning, health authorities must produce three Health Improvement Programmes each year.
- Implement Clinical Governance so that clinical practices can be closely monitored to ensure quality.
- A new Performance Management Framework must be designed to eliminate incorrect financial incentives.
- To improve and monitor the efficacy of patient treatment in accordance with national standards, a National Institute for Clinical Excellence will be established.
- Establishment of the Commission for Health Improvement to provide better health care.

Frank Dobson: Led the White Paper in publishing the New NHS: Modern, Dependable
- Tony Blair appointed Frank Dobson as the first Labour health secretary. Dobson was voted the best health secretary in a BMJ poll of leading medical people in 2013, despite admitting that he made a mistake in his career when he left to become Mayor of London in 2000.
The Impact of New Medicines in the NHS
- The NHS has been involved in the development of several medical and pharmacological processes since its inception. As a result, the UK’s health economy has grown significantly. The Office of Health Economics (OHE), a health institution, published a consultation study in August 2018 on the impact of several pharmaceuticals discovered over the NHS’s history on the UK’s health economics.
- The ten most important drugs brought into the NHS are as follows:
- ChlorpromazineIt was first used in the NHS in 1954. As the first antipsychotic, it was pivotal for the psychopharmacological revolution.
- Polio VaccineThe Polio vaccine was the NHS’s first immunisation programme, beginning in 1955.
- Oral ContraceptivesSince they became widely available in 1961, these drugs have had a significant impact on the health and economy of the United Kingdom.
- Second to Fourth Generation PenicillinDespite the fact that penicillin was discovered in 1928, years before the establishment of the NHS, the NHS facilitated its broad usage in the UK.
- Beta-BlockersBecause they lowered mortality and morbidity associated with heart failure, these drugs had a net beneficial fiscal impact on the NHS.
Beta2 Agonists
In the mid-1960s, 3 out of every 100,000 people aged 15-44 died of asthma, but this fell to 1 in every 300,000 after the introduction of salbutamol, the first beta2 agonist.
- TamoxifenTamoxifen was originally made available in the United Kingdom in 1972, and it was hailed as a turning point in breast cancer treatment.
- ImmunosuppressantsThe NHS worked on developing these after beginning with immunosuppressive drugs used in transplantation.
- HIV/AIDS AntiretroviralsThe first HIV antiretroviral was zidovudine. It averted a large number of AIDS patients from overwhelming the NHS.
- MMR VaccineThe introduction of the MMR vaccine aided the UK in dealing with the rising number of measles cases.
- The World Health Organization (WHO) considers all of them, with the exception of the MMR vaccine, to be ‘essential medicines’. To be regarded essential, a medicine must be one of those that meet a population’s primary health needs. This means it should be available at all times in every health care facility.
- The previously listed drugs made a significant contribution to the National Health Service, particularly in the United Kingdom, by preventing an increase in the number of instances of various ailments. As the number of patients decreased, so did the amount of money needed to sustain them. Another issue was that the growing number of patients could have produced a conflict in the capacity of the hospitals, which in turn could have had a detrimental impact on the programme. Furthermore, it had a substantial impact on the UK economy by increasing taxes and providing financial assistance to the NHS.