Key Facts & Summary
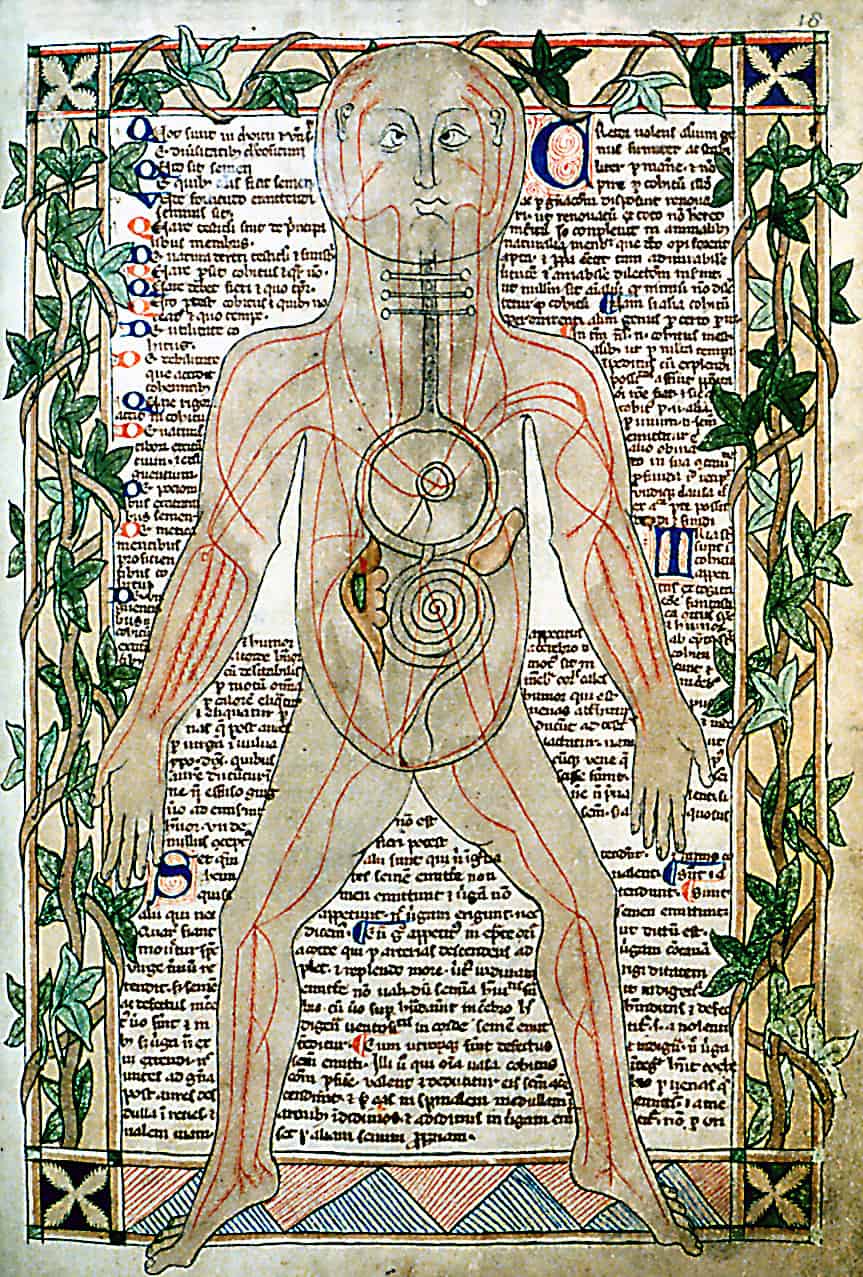
- Medical knowledge during the Middle Ages was derived from antiquity (in particular from Hippocrates and Galen).
- Medieval civilisations carried out medical practices that today are considered unhygienic, hazardous, and unreasonable.
- Looking back in time, one can be shocked when discovering the hygiene of our ancestors: fortunately, many of the practices mentioned below are no longer in use. However, it is nonetheless interesting to discover the way the generations that preceded us lived.
Overview
The superstition and dogmatism that marked the rise of Christianity in Europe continued to flourish throughout the Middle Ages. As in Babylon, astrology ruled the prognosis; diagnosis was largely limited to an inspection of the urine. Free inquiry, observation, experiments were out of question; learning, including magical learning, was devoted to the study of the ancient authoritative texts. Therapy relapsed into magic and prayer, fantastic and often revolting concoctions, charms and amulets, and faith healing. Venesection and various herbs were used widely. Dissection of cadavers was completely forbidden, and anatomy, if studied outside of textbooks, was based of the dissection of pigs. The root of the mandrake was surrounded with legends and was regarded as the sovereign remedy.
Hygiene and sanitation were at a very low level, since the human body was held in contempt. Saint Jerome saw no reason for any baths after the baptism. Tertullian thought that investigation was made unnecessary by the Gospel. And Gregory of Tour regarded seeking secular medical aid as blasphemy. The demonic theory of disease again gained ascendancy, or else, as in the case of the devastating plague epidemics, the blame was placed on the Jews.
It has been a recent tendency in the study of the history of medicine to regard the rise of the medieval medical school as a patch of light in the surrounding gloom of the Dark Ages, almost as a promise of the Renaissance. This view is debatable. Though the development of medical schools gave rise to a certain revival of Greek learning, acquired indirectly through the Arabic translations, it was the body of learning, and not its spirit that was revived. The canons of Hippocrates and Galen, Aristotle, and Avicenna, became the law, not their methods of research and observation.
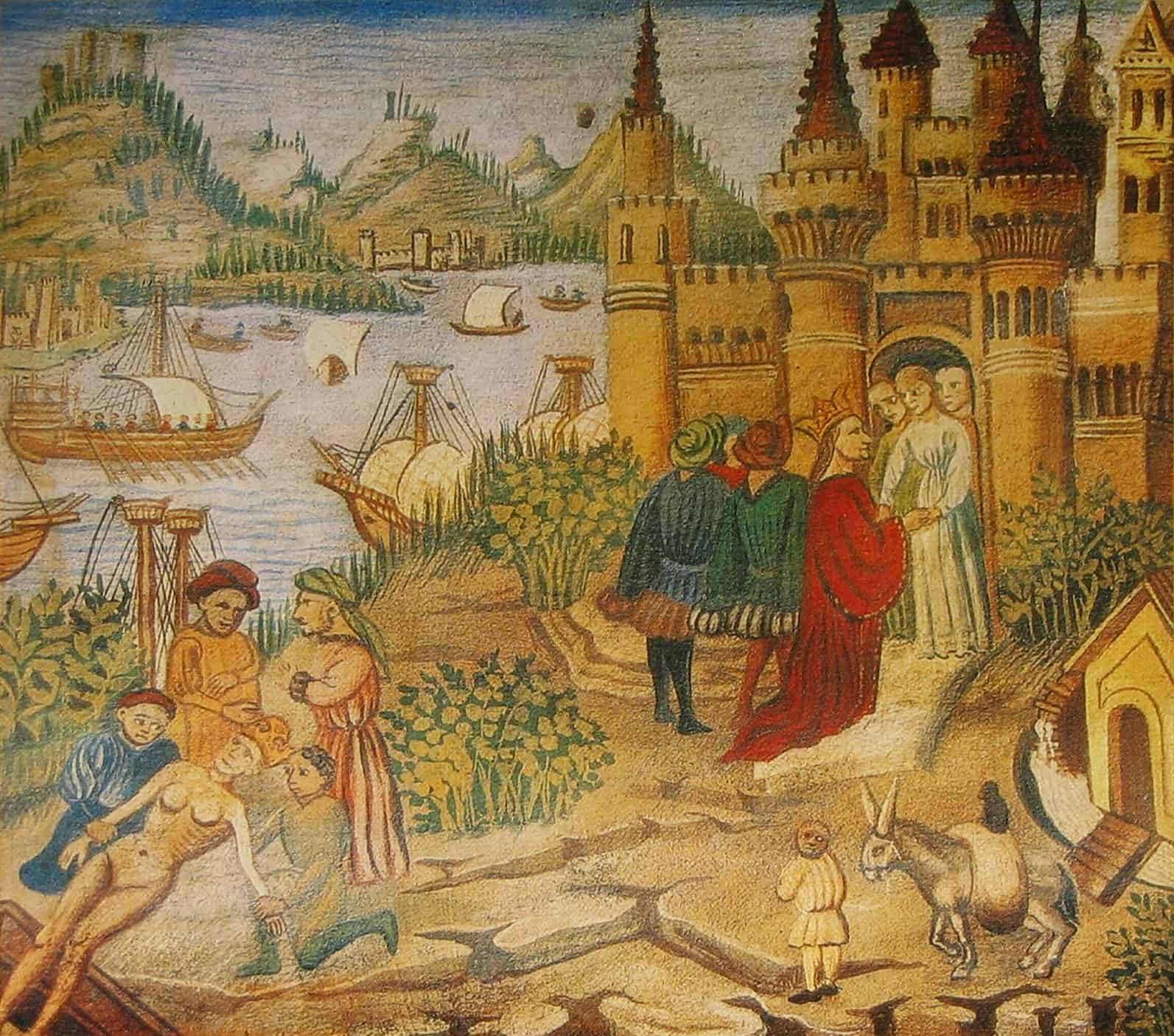
The famous School of Salerno which flourished from the X to the XIII century, was the first organised medical school in Europe. It was probably also the most enlightened. The Greek, Latin, Arabic, and Hebrew influences merged in Salerno, and it was known as the Hippocratic City The curriculum required three years of preliminary studies and five of medical; the graduate received the degree of Magister of Doctor, and the practice of calling a physician a ‘Doctor’ derives from Salerno. According to laws promulgated in 1240 by the Emperor Frederick II, a year of postgraduate practice under an established physician was required before the the graduate was licensed: ownership of an apothecary shop, or any business relation with an apothecary, was forbidden, and preparation of drugs was supervised by a inspectors.
The School of Salerno
The School of Salerno had many famous graduates. Its Regimen Sanitatis, a compendium of domestic medicine in the form of proverbs, was among the most popular books of the Middle Ages . Women were admitted to the School, but it is not certain whether as nurses, midwives, or physicians. For all its comparatively advanced character, Salerno still regarded suppuration as part of the natural wound healing, and its first textbook on anatomy was based on that of the pig. The connection of Constantinus Africanus (1010-1087) with the School of Salerno is uncertain, though he is known to have spent some time there and at the Benedictine monastery of Monte Cassino. Constantinus is known best for his extensive translations from the Arabic into Latin; in this way, he brought back to the West its lost Greco-Greco-Roman heritage. Subsequently Avicenna, Haly Abbas, and Maimonides, as well as Galen and Hippocrates, became entrenched in all the schools of the Medieval Europe.
After the decline of Salerno, at the end of the XIII century, the medical schools of Montpellier, Bologna, Padua, and Paris came into prominence, but their contribution to medical evolution was slight. Mundinus of Bologna dissected two cadavers, but he saw them through the eyes of Galen and Avicenna, and added nothing to the development of anatomy. The University of Paris outlawed surgical operations and clinical examinations. Arnold of Villanova, a celebrated teacher in Montpellier, invented alcoholic tincture of herbs, but he placed the diseases of women in his book on poisons, ‘since women are poisonous creatures’. Guy de Chauliac (1300-1367 AD), the most famous of medieval surgeons, was among the first to employ extensions for fractures.
Black Death
Throughout the Middle Ages, only the wealthiest could afford physicians. On the other hand, the poor were obliged to consult local practitioners that referred to folkloric traditions.
For most individuals, the lines between magic and medicine were blurred: medical practices resembled occult rites rather than practical cures. In fact, doctors sought to cure their patients through herbal remedies, concoctions, incantations, and charms.
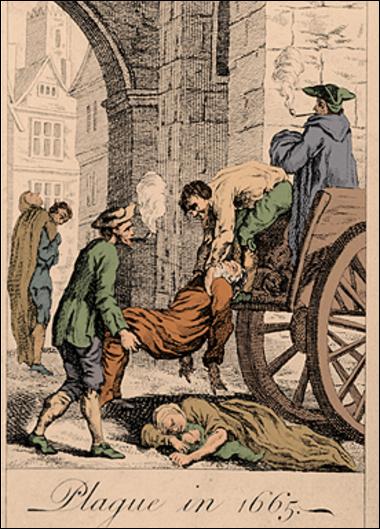
When the bubonic plague started in Europe due to the widespread unhygienic habits, people were not aware that the main cause of death was the bacteria Yersinis pestis, which was spread by infected rat’s fleas. Not having scientific explanation for the disease that had wiped out over one third of Europe’s population, people attempted to save their lives in a variety of ways. When the plague started manifesting in a person’s body, it would initially appear as a common flu with chills and feelings of weakness (Bardot 2019). It was necessary to tackle the illness within the first 24h of its contraction in order to destroy the bacteria. Failure to do so would result in it spreading across the lymphatic system before affecting the skin and internal organs. Subsequently, it caused ‘severe trembling accompanied by profuse sweating, subcutaneous haemorrhaging, and painful, dark reddish-purple spots rapidly developed. In addition, painful hypersensitive buboes formed in the lymph nodes of the armpit and groin. The buboes swelled as large as oranges, and filled up with pus and blood. If the buboes were not carefully lanced, the infection causes blood poisoning’, and further spreading of the disease happened when the buboes bursted (Bardot 2019).
Such a horrendous plague must have resembled a scene from a horrific gruesome movie, and in an age when religion ruled society and its thought, it is not surprising that the black death was considered a sort of divine punishment inflicted by God on the sinful members of humanity. In fact. some Christians that believed such theory punished themselves severely through self-flagellation.
Others thought that the best solution to avoid the plague was hiding in the sewers, were no one could reach them, see them, or touch them. However, the filthy conditions of the sewers, with their foul-smelling surroundings and fetid insects, did not save them from death: and although they may not have been infected by the bubonic plague, they nonetheless died due to other sever illnesses and infections.
The measures taken in order to avoid (or attempt to cure the plague) were ridiculous and often were the cause of death. In fact, some of these practices involved ‘drinking arsenic or mercury, not having thoughts about death in general, not having thoughts about the plague, not having sad thoughts, not eating figs, not eating meat, not running or walking outside, not exercising at all, not bathing, not sleeping in the day, and finally for good measure, not having sex’ (Sheriff 2013).
Richer people, on the other hand, ingested a crunchy mixture of crushed emeralds, and ingested the powdered stones either with a drink, or with food such as bread.
Aromatherapy was also employed, and individuals were encouraged to carry everywhere with them flowers with a sweet scent or herbs.
However, less hygienic practices were also in vogue. For instance, one practice involved cutting oped the buboes filled with pus and blood and applying a thick layer of…(wait for it..!) human excrements, resins, and flower roots. As if this was not enough, the concoction was wrapped tightly in order to be kept in place.
Others blamed the plague on the Jews, and believed that one of the ways to get rid of the plague was by killing them. Such an irrational decision to murder thousands of Jews was placated by Pope Clement VI who actively condemned the attacks and prompted members of the Church to protect them.
Other Medieval medical practices
If cures to the black death do not seem weird enough, the treatment reserved to the mentally ill during the Middle Ages was not any better. In fact, according to Tan (2016), those who were judged as mentally impaired, had their arms and legs tied up, meanwhile, their feet were plunged into salt water, their hair and nose were pulled, whilst pigs were squealing in their ears.
If an individual suffered from regular headaches, migraines, or epilepsy, trepanation was carried out: such practice consisted in perforating the skull with the intention of relieving pressure. However, such operations left the dura mater (i.e. the thick membrane that covers the brain) exposed to airborne bacteria, causing infections that could lead to death.
Teeth, on the other hand, were not treated with the utmost care and attention: not only were they cleaned with a cloth or with leaves, but also, in case of decay, they were extracted by local barbers. There was no such thing as a dentist!
Stomach problems were cured thanks to herbal remedies. One of them is St. Paul’s potion, which involved the use of several ingredients such as : ‘liquorice, sage, willow, roses, fennel, cinnamon, ginger, cloves, cormorant blood, mandrake, dragon’s blood and three kinds of pepper’ (Tan 2016). All these ingredients, played a part in the protection of a certain part of the body. For example, the liquorice was useful to ward off coughs and bronchitis; sage was useful for blood flow and increased memory; whereas ‘fennel, cinnamon, and ginger are carminatives that relieve the intestinal gases and a colicky stomach’ (Tan 2016).
On the whole, during the Middle Ages, very little was added to medical knowledge.
Bibliography
[1.] Bardot, J. B. (2019). Garlic kills Bubonic Plague and other pathogen -based Disease Epidemics. Available from: https://www.jbbardot.com/garlic-kills-bubonic-plague-and-other-pathogen-based-disease-epidemics/
[2.] Bovey, A. (2015). Medicine, diagnosis, and treatment in the Middle Ages. British Library. Available from: https://www.bl.uk/the-middle-ages/articles/medicine-diagnosis-and-treatment-in-the-middle-ages#
[3.] Goldiner, S. (2012). Medicine in the Middle Ages. Met Museum. Available from: https://www.metmuseum.org/toah/hd/medm/hd_medm.htm
[4.] Horder, P. (2011). What’s wrong with Early Medieval Medicine? Social History of Medicine. 24 (1). Pp. 5-25.
[5.] Murrell, D. (2018). What was medieval and renaissance medicine? Medical News Today. Available from: https://www.medicalnewstoday.com/articles/323533.php
[6.] Shariff, M. (2013). Ten Crazy cures for the Black death. Listverse. Available from: http://listverse.com/2013/01/21/10-crazy-cures-for-the-black-death/
[7.] Tan, L.A. (2016). 6 Horrifying and weird Medieval medical practices. Available from: https://today.mims.com/6-horrifying-and-weird-medieval-medical-practices
Image sources:
[1.] https://upload.wikimedia.org/wikipedia/commons/0/01/Blood_letting.jpg
[2.] https://upload.wikimedia.org/wikipedia/commons/1/12/13th_century_anatomical_illustration_-_sharp.jpg
[3.] https://upload.wikimedia.org/wikipedia/commons/a/a4/ScuolaMedicaMiniatura.jpg
[4.] https://upload.wikimedia.org/wikipedia/commons/1/1e/Great_plague_of_london-1665.jpg